West Hill is a quiet neighbourhood nestled between the branches of the Highland creek in east Scarborough, bounded by the elite Scaroboro Golf and Country Club to the west and Lake Ontario to the south. In the 1950s and 60s, middle-class families drawn by the area’s affordable houses and rural beauty turned the community into a post-war suburb. Along Kingston Road, which cuts through the neighbourhood, motels and plazas served drivers passing through towards Toronto.
When the 401 was built north of the neighbourhood in 1968, however, West Hill’s businesses began to lose customers to those along the expressway. By the 1990s, many of the motels were run-down and some were converted into shelters. Around this time, dense townhouse complexes and affordable high-rise units began to be built.
Drive across West Hill today, along the pretty tree-lined section of Lawrence Avenue East, and you’ll see post-war bungalows juxtaposed with townhouses and high-rises from this second wave of development. Many of those living in the bungalows raised their families here and are now elderly. Those living in the apartment complexes are working hard to build a life for their young kids, but with growing challenges. According to data from the city of Toronto, 40 percent of kids who live in West Hill are classified as low-income, well above the Toronto average of 26 percent. Many are navigating cultural and language barriers, with Tamil, Tagalog, and Bengali as the top non-English languages.
One challenge is simply finding health care. West Hill has around 2.5 doctors providing comprehensive primary care services per 10,000 residents. Compare that to the 31 comprehensive primary care physicians per 10,000 in Bayview Village, a high-income residential neighbourhood in north Toronto, or the 58 in Playter Estates, an exclusive enclave north of Danforth and east of Broadview.
Having few primary care doctors working in a neighbourhood isn’t necessarily a problem. In areas full of young and healthy people, having fewer doctors is expected and appropriate. But the population of West Hill has complex health problems. The neighbourhood’s SAMI score (which measures the complexity of patients) is the 19th highest of Toronto’s 140 neighbourhoods. Dr. Avnish Mehta, who works at a Community Health Centre north of West Hill, says he has many patients who come from the neighbourhood and travel by TTC to see him. “I have patients who don’t follow up as often as I would like them to because of travel. I think that’s pretty universal within Scarborough.”
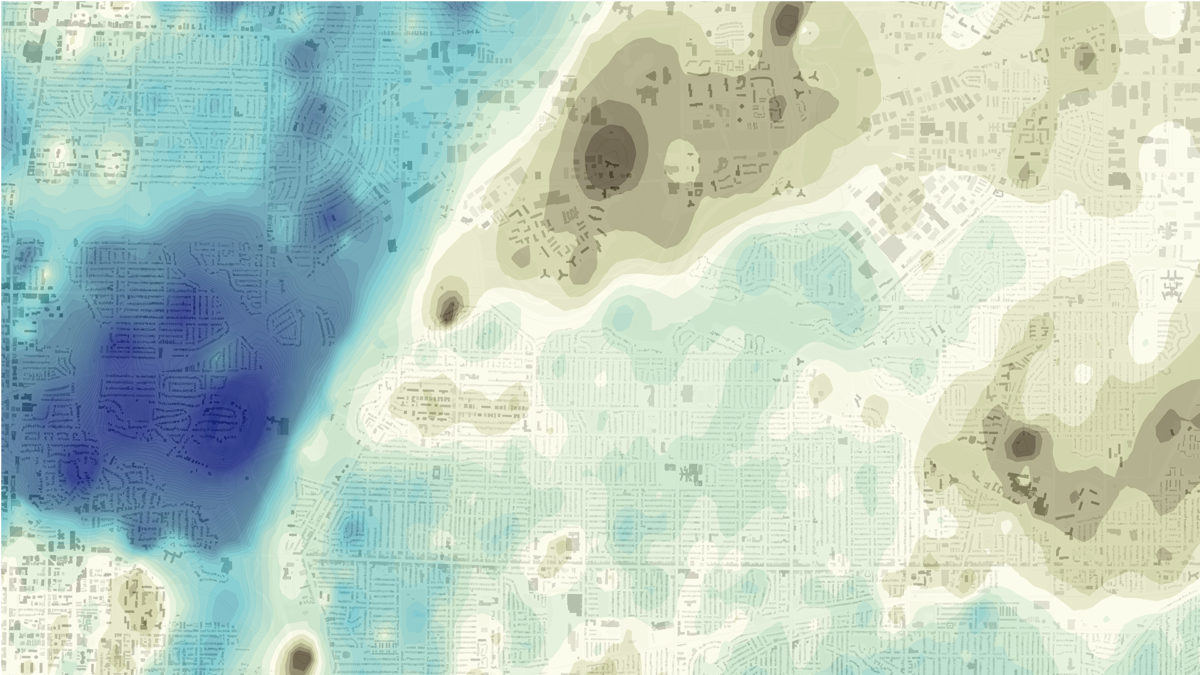
West Hill is far from the only neighbourhood in Toronto where needs are high and access to primary care is dismally low. If you look at a map that overlaps SAMI score and physicians per 10,000 people, a clear pattern emerges. High needs/low access areas are concentrated in Scarborough and in the city’s northwest suburbs surrounding the Humber River. Sadly, and perhaps unsurprisingly, these areas correlate with the map of income distribution. In other words, the poorest Torontonians with the greatest health care needs have the fewest options.
We hear a lot about food deserts, urban neighbourhoods where fresh fruits and vegetables are hard to access. Maybe it’s time we talk about “health care deserts” too. And in a publicly funded system, it’s worth asking why health care deserts exist in the first place. Why aren’t the doctors where the sick people are?
How do health care deserts happen? The biggest reason is that most doctors are “small business people locating their businesses where they choose,” explains Dr. Rick Glazier, a family health physician at St. Michael’s Hospital and a senior scientist for Ontario’s Institute for Clinical and Evaluative Studies. Doctors want to set up their businesses near where they live, and doctors want to live in high-income, walkable neighbourhoods. Health care services have therefore followed a larger demographic trend, as upper-income people increasingly choose to stay in the city core.
Funding models also play a big role in where a family doctor locates. Ontario, like many provinces, has been moving to a “team” model for health care in which physicians refer patients to allied providers, including dieticians, physiotherapists and counsellors, who all work under one roof. Comprehensive models include Family Health Teams and Community Health Centres, which are mandated to serve the most vulnerable and are often located in underserved neighbourhoods. Because they’re expensive, however, the government simply doesn’t fund enough of them; they serve fewer than four percent of Ontarians. Meanwhile, Family Health Teams, which serve 25 percent of Ontarians, appear to be concentrated in more affluent areas of the city. There are far more in downtown Toronto than the inner suburbs.
“I worry about my patients not getting the care and monitoring they require when they move away from downtown”
Family Health Teams were created when doctors proposed them and the Ministry of Health and Long-Term Care approved them. Between 2005 and 2012, close to 200 Family Health Teams were created in Ontario, including 21 in Toronto, through an application process which has since been closed. Doctors in the inner suburbs haven’t worked to set up Family Health Teams because the model doesn’t work out financially for them, argues Glazier. Family Health Teams remunerate physicians for each patient they have on their roster. So a downtown doctor with a roster of 1,600 will be paid far more than an inner suburb doctor who only sees 1,000 patients because each patient requires more support.
Because teams aren’t financially attractive for doctors in high-need areas, doctors in these areas are often left working without the supports seen in other parts of the city. “You end up with a primary care provider who is overwhelmed with very complex patients with very complex social determinants of health,” explains Dr. Onye Nnorom, associate program director of the Public Health and Preventive Medicine Residency Program at the University of Toronto.
Dr. Ritika Goel, a family physician with Inner City Health Associates who works with homeless and marginalized populations, says her patients have been turned away in underserviced neighbourhoods because the overwhelmed nearby doctors can’t take on a high-needs patient. Once her homeless patients are housed, usually in low-income parts of the inner suburbs, she fears for their health. “I worry about my patients not getting the care and monitoring they require when they move away from downtown,” she says.


A “health care desert” doesn’t merely mean an area with lower access to primary care, but to specialists too. And here, again, the people who have the highest health needs often have the least access to care. A 2018 report by ICES mapping the number of specialist visits per 1,000 population shows that lower income areas in the northwest and northeast have the least specialist visits. That’s likely because they’re difficult to access and wait times are longer. Downtown, there are several hospitals right next to one another. In the northwest region, it can take over an hour to travel by transit to the hospital in your catchment area, says Dr. Ralph Masi, a family doctor who practices at Wilson and Keele. It can take a year for Masi’s patients to see a psychiatrist, though his colleagues downtown get their patients to a psychiatrist within a couple of months.
One of the northwest areas with the lowest numbers of specialist visits is Black Creek, the neighbourhood north of Jane and Finch. The average household income there is around $47,000, compared to the city average of $66,000. The neighbourhood also has double the rate of refugees compared to Toronto as a whole. Victoria, a refugee from Nigeria and a former personal support worker, lives in a two-bedroom apartment in Black Creek with her teenage son and daughter. She has multiple health issues, many of which stem from a car accident several years ago. She’s had several surgeries, including knee replacements, and she has high blood pressure and glaucoma, which has robbed her of 50 percent of her vision. Her orthopedic surgeon is a 15-minute drive away from her apartment, and her ophthalmologist is 30 minutes away. She has to take cabs. She can’t take TTC, because she uses a walker and she finds Wheel Trans service unreliable, which doesn’t work when you need to be on time.
More often than not, she doesn’t go to her health appointments. “I’ll choose the one that I think is most important and I’ll cancel the others,” she says. “What else can I do?” Her family of three lives on $1,330 a month, from the Ontario Works social assistance program, and her rent alone is $1,080. If she were to make all of her appointments, cab fare would eat up a significant portion of an already lean budget.
People like Victoria, who have poor access to health care, suffer for it. A study that examined data from more than 3,000 US counties, published just last month, showed those who lived in areas with fewer primary care physicians died sooner than those with greater access, and the income and education levels of the patients didn’t explain the discrepancy.
When a patient has to travel more than an hour for an appointment, they often end up delaying the tests or treatments. Dr. Gary Bloch, a family physician with St. Michael’s Hospital and Inner City Health Associates, says patients who travel a long way to see him are frequent no-shows. “The TTC fare is too expensive, or they have really significant competing priorities in their lives, like finding food or taking care of their kids, and they can’t afford the four hours back and forth,” says Bloch. Patients living in health care deserts often end up seeking care for only the health issues that have become so bad they simply can’t be ignored any longer. Needless to say, prevention services, like cancer screenings, tend to fall to the wayside.
The gaps in our system won’t go away easily. A system where health services are located where they’re most needed, “takes a fair bit of organizational planning, and a strong population health approach and that’s not something we’re big on,” says Masi.
To address health care deserts, medical schools could send more residents to low-income and underserved communities, because doctors are more likely to practice where they train. (Residency training spots are currently concentrated downtown, near hospitals and universities). They could increase funding to the largely stalled Community Health Centres, which have a mandate to provide holistic services for the most disenfranchised. The funding incentives for Family Health Teams could encourage, rather than discourage, doctors to set up comprehensive teams in areas of high need. That’s assuming that the government opens up the application process, which has been frozen since 2012.
Those ideas may sound expensive, but studies show investments in primary care also save costs, by reducing the use of hospitals and acute care. For almost all health issues, from diabetes to schizophrenia to pregnancy, early intervention prevents expensive-to-treat complications. Health care deserts are further increasing existing inequities, making it even harder for people already struggling with low income, disability, racism, and more. It’s time for our health system to tackle them head on.