At age 77, Ellen Lamb was living comfortably on her own in a 14th-floor apartment at Bay and Bloor St. She often met friends for coffee nearby and visited the City Market on Fridays to pick up groceries. Once a week, she brought her laundry up to the laundry room on the 30th floor of her building to do it herself.
All that changed in January 2023, when Lamb collapsed in her apartment from a bleeding stomach ulcer. A neighbour noticed her apartment door was ajar, but didn’t think it warranted alerting the building’s security staff until 12 hours later.
Lamb had lost a lot of blood. When she was brought, unconscious, to a hospital emergency department, she had a heart attack while waiting.
The emergency team performed chest compressions and intubated her. They saved her life, but in doing so, added to her injuries. The chest compressions broke her ribs. Being hooked up to a ventilator led to complications, since she had a pre-existing lung condition. She also suffered a broken vertebrae in her neck.
After more than three months in hospital, Lamb was transferred to a Toronto rehabilitation hospital in early May. She was still relearning how to walk when the time came for her to be discharged. She didn’t feel ready to leave yet, neither physically nor logistically, but hospital beds are scarce across Ontario, and she had been there nearly two months already. Someone else needed her spot.
Before her collapse, Lamb used a walker to get around. Now she needed a wheelchair. She couldn’t safely stand up on her own without supervision, and she was unable to use her right hand, which she had injured when she fell.
So she couldn’t return to living by herself in her apartment. She needed somewhere to live where help would be close at hand. But securing a spot in a long-term care home wasn’t an option either—at least not within the timeframe that Lamb was scheduled to be discharged. The median wait time to move into a long-term care home for Ontarians in hospital is 72 days. For those living in the community, it’s 201 days.
With the help of her daughter, and after a frantic scramble, she landed an apartment at a retirement home in July. She could receive publicly-funded home care services, but would have to cobble together whatever additional care she needed through paid services.
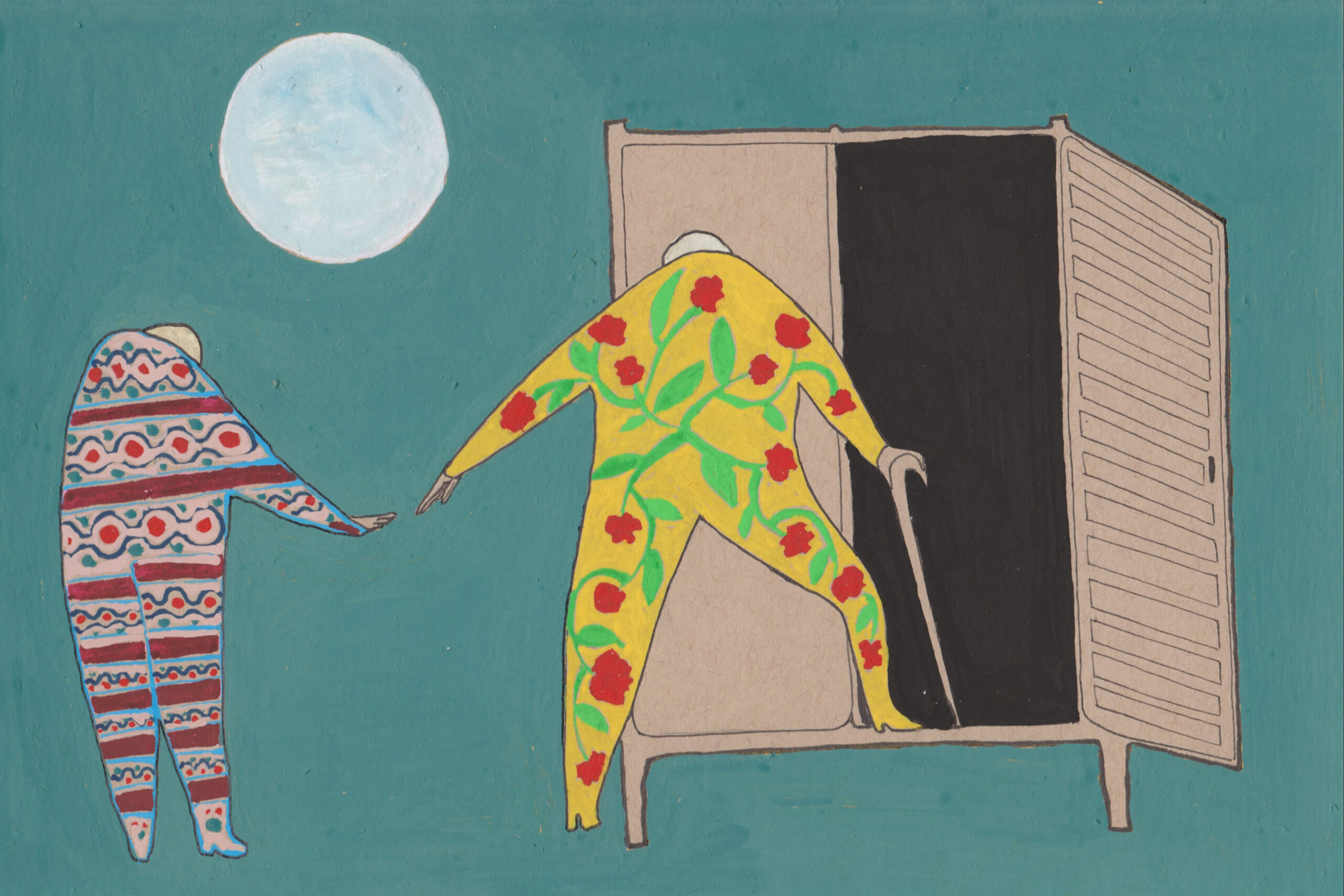
And thus, Lamb has found herself, as she put it, in “the eye of a hurricane,” observing the various ways in which home care works in Ontario—and the ways in which it fails.
“I think the systems they’ve put in place, sometimes they work and sometimes they don’t,” she says, selecting her words carefully. She squints through her large glasses as she considers how best to describe her experience so far with home care. She doesn’t mean to complain.
“I don’t know,” she says finally. “As I’m thinking about this, they seem to have a hard time figuring out individualized care.”
In other words, the home care that Lamb and others receive isn’t necessarily the home care they actually need.
Roughly one in six Torontonians is now over the age of 65. And many are in Lamb’s position, just illness or one health incident away from losing their ability to live independently.
When that happens, home care should be the answer, allowing those who wish to do so to remain in the comfort and privacy of their own homes. It’s what most people want, and what the government has long indicated is the way forward to ease the pressure on overburdened hospitals and long-term care homes. Yet home care has never lived up to its promise. It’s chronically underfunded, with underpaid workers in short supply. It’s difficult to navigate, seemingly designed for the companies that provide care services instead of the people they’re serving. And it’s an opaque and confusing black box that too often leaves recipients and their families without answers to their most basic questions: What services are they eligible for? Who will come and when? Who is accountable?
Late last year, the province introduced new legislation that will reorganize how publicly funded home care is managed in Ontario, promising to make it easier for people to find and navigate home care services. But the devil is in the details, with some health care researchers and advocates worried the new reforms will amount to little more than rearranging deck chairs, or, worse, will further erode the quality and public accountability of home care.
If the government intends to fix the flaws in publicly funded home care, now is a critical time. At stake are the wellbeing and quality of life of a large cohort of Ontarians who are facing the day they will need help caring for themselves. Without adequate and appropriate home care, they risk being driven into long-term care, which itself is overburdened, understaffed and insufficient to meet demands. Or they may be forced to struggle at home, relying on family caregivers if they have them, or languishing largely on their own if they don’t.
Join the thousands of Torontonians who've signed up for our free newsletter and get award-winning local journalism delivered to your inbox.
"*" indicates required fields

It would be inaccurate to describe home care in Ontario as a system. It’s more of a patchwork of services that includes everything from professional care, such as physiotherapy and nursing, to personal support, like assistance with bathing and getting dressed, to homemaking. Today, publicly funded home care is delivered by a mix of for-profit and not-for-profit service providers. Many of these providers, along with a broad marketplace of private operators, also offer their services privately to those who are able to pay for them, sometimes as much as $40 an hour for personal support.
When it began, home care in Ontario was an entirely not-for-profit phenomenon. In the late 1890s, the Victorian Order of Nurses (now VON Canada) was established as one of the first organizations in the country to provide home nursing.
Throughout much of the twentieth century, home care remained largely an ad hoc, non-profit service, provided by municipalities and organizations like the Victorian Order of Nurses, the Visiting Homemakers Association (now VHA Home Healthcare) and Saint Elizabeth nurses (now SE Health; note that SE Health is a financial supporter of The Local but had no role in the conceptualization, review, or editing of this story).
The first publicly funded home care program was formally established by the province in 1970.
In 1994, nearing the end of its mandate, the New Democratic Party government passed legislation to modernize home care. Under the Long-Term Care Act, government-designated multi-service agencies were meant to provide a range of services, from meal and transportation services to nursing and occupational therapy. The stated aim was to coordinate these services with those offered by hospitals and other parts of the health care system to promote a continuum of care, allowing people to age in their homes and communities. How this system would have panned out, though, Ontarians never got a chance to find out.
Instead, in 1996, the provincial government, under then-Premier Mike Harris, opened the home care market in Ontario to for-profit providers, allowing companies, both for-profit and not-for-profit, to bid for contracts. These contracts were awarded by 43 regional Community Care Access Centres, or CCACs, that the province established.
Introducing competitive bidding allowed for-profit providers to squeeze out many not-for-profit providers, to the ire of critics who argue profits come at the cost of better wages and quality of care. Additionally, a new set of challenges emerged.
In the early days, contracts were relatively short, and every time one was awarded to a new provider, it caused chaos in the labour force, says Natalie Mehra, executive director of the Ontario Health Coalition advocacy group. Staff would be laid off en masse from the previous contractor, while the newly awarded company, needing to quickly ramp up its pool of workers, would then hire them anew. Yet for these workers, starting with a new employer resulted in a loss of seniority and things like accrued vacation. Many workers simply left the sector as a result, Mehra says, and the labourforce has never recovered
The Liberals later put a halt to these recurrent upheavals with a moratorium on competitive bidding. Since then, many of those contracts, which award providers a certain volume of services within a geographic area, have remained in place. (According to its website, the HCCSS works with more than 150 service providers via roughly 400 contracts, though by some estimates, the vast majority of home care in the province is provided by nine large providers.) But some key issues, including a severe labour shortage, a lack of public accountability and a lack of focus on patient- and family-centred care, persist.
In the decades since, home care has been orchestrated by an alphabet soup of acronym-named agencies and organizations. There were the CCACs, which were later amalgamated and each aligned with a crown agency called a Local Health Integration Network, or LHIN, which, in turn, were renamed Home and Community Care Support Services, or HCCSS.
Today, it’s these HCCSS organizations—a total of 14 of them in Ontario—that coordinate most of the publicly funded home care in the province.
“If you think this system looks like a sea of acronyms that are completely incomprehensible to any normal person, it’s because it is,” Mehra says. “Because the whole system has been set up to serve the provider companies, not the public.”
To home care recipients like Ellen Lamb, it arguably matters little which combination of letters manages their care. As Dr. Paul Holyoke, vice-president of research and innovation at SE Health’s SE Research Centre, explains, the names have changed over the years, but the structuring of home care has, for the most part, stayed the same.
What’s important to note is that since the Harris government, home care has largely been paid for per service, rather than according to the level of care that a patient needs. On paper, any one visit is worth the same as the next; every personal support worker is the same as every other personal support worker; every nurse is the same as every other nurse.
One result of this is that clients can wind up with a revolving door of different carers, sometimes from different provider companies. Currently, if the HCCSS determines a client needs two visits from personal support workers over two weeks, Holyoke says, one provider company may have enough staff to cover one week, while another may take on the second.
At 6:00 a.m., Lamb wakes up in her bedroom at the retirement home where she’s been living since she left the hospital.
It’ll be at least two hours yet before a personal support worker arrives to help her out of bed. So Lamb lies there. Sometimes she dozes off. Sometimes she picks up her mobile phone and reads The New York Times online. She waits.
Eventually, someone from the publicly-funded home care agency will come. Maybe it will be the same personal support worker who has been coming for the past Wednesday, Thursday and Friday mornings.
But who knows? Maybe it will be someone new. In that case, Lamb will have to go over her routine and provide instructions yet again about the care she needs—how to help her with the bathroom, how to prepare her breakfast, how to put in her hearing aid.
Lamb isn’t clear who made the decision or how, but sometime before she was discharged from the rehabilitation hospital, someone decided she would get three visits a day from personal support workers through provincially-funded home care from a non-profit agency. She also gets a fourth, shorter visit every evening from a home care nurse to help her take her medication.
If she had her preference, she’d get that third personal support worker visit at night to help her get back into bed. But since she was informed that no one at the agency works past 6:00 p.m., that third visit typically happens in the late afternoon. She pays her retirement home to send one of their personal support workers to assist her for bedtime at a more reasonable 9:30 p.m.
The one home care nurse who comes regularly is wonderful, Lamb says. The medication he helps her take requires a nebulizer, which is a little machine that converts the liquid medicine into vapour she inhales. He’s pleasant and reliable and knows what to do. But occasionally, the agency has sent nurses who have never used a nebulizer before. When that happens, here we go again; Lamb has to coach strangers how to take care of her.
For the most part, she likes the carers who come, but she finds it hard to adjust to the parade of people who enter her home at unpredictable hours. A “cast of characters,” she calls them.
“I’m tired of it,” she says. “I’m very tired of it.”
She has tried to ask for a weekly schedule, so she can at least have some sense of whom to expect and when. But as she’s discovered, “That’s sort of impossible.” When she tried calling the agency, it went straight to voicemail, and no one called back.
Typically, an HCCSS care coordinator assesses a person’s needs, develops a care plan for them and connects them with service providers to provide the care in their homes. The coordinator also gives them information about other community support services they may need. Lamb doesn’t recall meeting an HCCSS care coordinator, nor has she received her care plan, either from the HCCSS or the agency tasked with delivering her home care. If there is a plan, she says, it doesn’t feel that way.
“All they do is assign people to come in,” she says. “But it’s not cohesively thought through.”
In this way, Lamb’s metaphor of finding herself in the eye of a hurricane is fitting. It’s as though she’s a passive subject of her own care. All the decision-making and coordination happens around her, without her say.
Lois Reimer, 91, encountered some similar issues when she received publicly funded home care prior to moving into long-term care about two years ago. Although she describes her experience as generally positive, one of the main reasons Reimer, who uses a wheelchair, decided to enter long-term care was because she couldn’t get help overnight. With home care, once she was helped into bed, she couldn’t get up again on her own.
“So I was sometimes in bed from about seven in the evening to about 11 in the morning,” she says. That’s 16 hours in bed, alone.
“The whole system has been set up to serve the provider companies, not the public.”
In October, in tacit acknowledgement that home care needs fixing, the Ontario government unveiled Bill 135, the Convenient Care at Home Act, which received Royal Assent in early December. This move will dissolve the HCCSS. The province will create a new organization, called Ontario Health atHome, that will coordinate all of the home care services across the province. Meanwhile, something called Ontario Health Teams, which are groups comprising for-profit and not-for-profit health care providers including hospitals, doctors, and home and community care providers, will be responsible for connecting people to home care services, starting in 2025.
According to the province’s description, “Ontario Health Teams will be a one-stop shop that provides people with easy-to-understand home care plans,” and home care will be convenient and easier to navigate.
Reducing frustration for users sounds good, in theory. Depending on how this actually translates into practice, this reorganization could be a chance to significantly improve home care in some respects. One possibility is adopting the kind of “bundled care” model that’s currently used by some hospitals to help patients recover at home over a set number of weeks after they’re discharged. Instead of being paid by visit, contracted service providers generally receive payment to cover all the necessary home care a patient may need for the set period. Under this model, the focus tends to be more on patient outcomes instead of the number of visits providers need to fulfil.
From the perspective of the Ontario Health Coalition, however, the new Act amounts to the further privatization of home care, a continuation of the government’s move to privatize other parts of the health care system. Natalie Mehra from the Ontario Health Coalition predicts the new changes pave the way for the province to hand over the contracting and subcontracting of home care services to provider companies themselves. Already, the administration of home care lacks oversight and democratic accountability, without publicly elected board members and accessible minutes, she says. “This new Act is the one that actually completes the process…to privatize the last remaining public parts of home care.”
There’s another reason to question whether the latest reform will meaningfully improve home care: notably absent from the government’s promises is any mention of actually increasing people’s access to home care or the quality of care.
Further privatization could make it harder to ensure provincial money goes toward making these improvements. When home care is contracted out to providers that don’t answer to the public, it can be difficult for the public to keep an eye on how they’re using taxpayer dollars. A 2015 report from the Office of the Auditor General of Ontario found 82 percent of the funding that not-for-profit and for-profit service providers received from CCACs was spent on direct patient services, while 5 percent went to profit. But it included an important caveat; these findings were based on financial information that providers voluntarily submitted to the auditor general’s office. “Because we do not have the legislative authority to directly audit the contracted private-sector contractors that sold services to the CCACs, we were not able to perform audit procedures to verify the accuracy of this information,” the report said.
A separate report, published the same year by a Ministry-appointed expert group, stated there was too much variability in access to home care services across the province, and too little accountability for the performance of service providers. That report, titled “Bringing Care Home,” also pointed to a need for home care in the province to be delivered in a way that puts the interests of clients and their family caregivers first.
Dr. Samir Sinha, director of geriatrics at Sinai Health and University Health Network and director of health policy research at the National Institute on Ageing, was a co-author of that report. Nearly a decade later, a lot of those fundamental issues remain and home care still operates much in the same way, he says.
Government spending on home care is also insufficient to meet the needs of the growing aging population, Sinha adds. Case in point: the Financial Accountability Office of Ontario has estimated that the province’s plan to increase investment in home care would amount to older Ontarians getting the same amount of funded hours of nursing and personal support in 2024-25 as they did five years prior.
“Whenever you are trying to access home care, it remains quite limited,” Sinha says. “A lot of my patients just can’t get what they need to be able to go home from hospital or to be able to stay at home in the community.”
Adding to this problem of limited access, a shortage of workers has only gotten worse over the years, says Mehra, to the point where, if a worker is ill or there’s simply no one available, “no one shows up at all.”
And when that happens, there are no repercussions to the provider company, she says—at least none that can easily be found. “If they can’t fulfil the contracts, there’s no real accountability.”
One of the reasons this labour shortage persists is that health care workers are more likely to seek employment in hospitals or long-term care, where they’re paid more, Sinha explains. A personal support worker typically earns $5 an hour less in publicly funded home care than in a publicly funded long-term care home, he says. And at a publicly funded long-term care home, they’re likely to earn $5 an hour less than in a publicly funded hospital.
It’s not yet clear if or how the new home care reforms will tackle these issues. The Ministry of Health did not respond to The Local’s requests for an interview.
To begin to understand who the key actors are in Ontario’s home care sector requires extensive research. Megan Linton, a doctoral student in sociology and political economy at Carleton University, and her team have spent about 10 months so far, attending workshops, meeting with major stakeholders and researchers in the field, and painstakingly scouring company information to create maps of the various service providers, who owns and runs them, who funds them, and how they relate to each other. The fact that such an exercise requires considerable investigation on her part, “really shows how complicated and obfuscated the system is,” says Linton, whose work is part of a research project called Towards Just Care.
Although her work is still in progress, a preview reveals a web of more than a dozen not-for-profit providers, such as VHA Home Care and St. Joseph’s Home Care, and for-profit providers, such as Spectrum and Paramed, as well as some of the companies and organizations that are linked to them. For example, a line on one of her maps shows Paramed is owned by Extendicare, one of the biggest owners of long-term care homes in Canada. Another line shows the not-for-profit provider Acclaim Health receives funding from the United Way.
The purpose, she explains, is “to expose who actually is at the centre of this,” when, for home care workers and recipients, their main points of contact are with each other.
In spite of her digging, there are important aspects of home care that remain a mystery, Linton says, such as how much money the government is giving various organizations for their services and how many hours of service they’re meant to provide, since this is excluded from certain Freedom of Information legislation.
Workers themselves don’t always know who’s paying for the services they provide.
Vilma Baptista worked part-time as a personal support worker for three home care providers, Bayshore, We Care, and Home Life Care Services, for close to two decades. To supplement her income as a hotel housekeeper, she would give the companies her availability and pick up about 10 to 16 hours a week from them.
When visiting clients, she didn’t always know whether the work was publicly funded or paid by the clients privately. “They don’t tell you,” she says.
She earned less working at the hotel than she did as a personal support worker, but the hotel provided greater income security and benefits.
Owing to her limited weekly hours as a personal support worker, Batista didn’t experience burnout herself, though some of her colleagues certainly did. She suspects they simply had too many people to take care of.
“They have a heart, right? But they don’t have time…to give what they can,” she says.
Batista is originally from the Philippines and immigrated to Canada in 1989 from Saudi Arabia, where she worked as a domestic worker. Although she retired in 2021, she continues to provide home care to a single client through a private agency. The work amounts to about four hours a week, and she needs the extra income. She owns a house and a car, but is still paying off her mortgage. She has no family in Canada, and can’t afford to sponsor her family in the Philippines to come here.
Now 69, she says she worries about her own future as she grows older, and the futures of her colleagues, too. They’ve provided care for so many people throughout the years. Who will take care of them?
Notably absent from the government’s promises is any mention of actually increasing people’s access to home care or the quality of care.
If the province truly intends to make meaningful improvements to home care, it has no shortage of ideas from which to draw. In the 2015 “Bringing Care Home” report, the first recommendation Sinha and his co-authors presented was for the Ministry of Health to endorse and incorporate the principles of client- and family-centred care. That means a paradigm shift that would, among other things, treat clients’ families as equal partners in their formal care team, have a single care coordinator work with a client and their family to determine the most appropriate services for their needs, and ensure clear and regular communication with the care coordinator.
Another of their recommendations was to have the Ministry explicitly define a “basket of services” so that clients and their families can know which services they can expect, and under what circumstances. Without this information, they continue to be left in the dark. “It’s not very transparent how people are assessed, and who gets what,” Sinha says.
The advocacy group Seniors for Social Action (Ontario), meanwhile, has been calling for more government spending on home care. Dr. Patricia Spindel, chair of the advocacy group, expressed frustration over the extent to which institutionalized care tends to get prioritized over home care. In contrast to the more than $6 billion the province promised to build more long-term care, she noted, they have pledged just an additional $1 billion toward home care. Furthermore, it hasn’t addressed wage parity for workers, she added.
In the meantime, her group frequently hears from people about their struggles to get adequate home care.
“Most, if they’re lucky, they can get four hours a week, and they have to fight for that,” Spindel says. In the worst case, some have mentioned they’re eyeing Medical Assistance In Dying (MAID). They’re “saying, ‘Just let me die… I don’t want to be abandoned here by myself, so you know, no one finds me,’” Spindel says.
Beyond the fact it’s what people want and need, there’s also a financial and health care efficiency case to be made for investing more in home care. A 2022 report from the province’s largest home care organizations cited costs of about $730 a day to care for a person in hospital, $201 in long-term care, and $103 in home and community care.
“Strong home care is a crucial underpinning for a well-functioning health care system,” the report said. It added: “There is no alternative but to get it right this time.”
For Mehra of the Ontario Health Coalition, this doesn’t mean home care should be seen as a replacement for other forms of care. Rather, she emphasizes, Ontarians need a range of care they can depend on.
“Not everyone is happy living independently,” Mehra says. “You need home care and community care. You need supportive housing. You need long-term care homes and you need hospital care.”
The other day, one of Ellen Lamb’s personal support workers informed her she’d be off work for a few weeks. She told her the agency would arrange for someone to come in her place and was surprised when Lamb said the agency hadn’t called her, not even to return her messages.
The next morning, a new personal support worker whom Lamb had never met eventually showed up. But by that time, it was already around 10:30 am, and tired of waiting without knowing whether anyone would arrive, Lamb had asked her retirement home to send one of their workers to help her out of bed.
Asked about the future, Lamb says she tries not to think about that. “I don’t know how to plan for it,” she says, explaining she doesn’t have unlimited money. She knows other people who are homeowners sell their houses for a good price, which allows them to live well in seniors’ residences later in life. “That is not my story.”
Instead, she’s focused on becoming more independent again by practising the exercises she’s learned through physical therapy and occupational therapy. She can walk back and forth in the corridor outside her apartment, and over time, has increased the distance she can cover. Even so, she admits she may have hit a plateau in her recovery.
And so, Lamb waits. She waits for the next person to arrive to help her get in and out of bed. She waits for communication from the agency. She waits for the province to finally ensure Ontarians receive adequate and appropriate home care. Here, in the eye of the hurricane, there is little else one can do.