
Three weeks ago, Maria Isabel Gilbert felt so exhausted she needed to lie down on the couch. Over the next few hours, she developed a fever. The next few days brought a headache, dry throat, diarrhea, and chills. “I thought, ‘Oh boy, this is it,’” says Gilbert. This, of course, being COVID-19.
Gilbert is a personal support worker (PSW) who provides care for seniors, most of whom have limited mobility and live in apartments, condos, and houses. She typically visits about six homes a day, helping with bathing and meals, providing medications, throwing laundry in a machine, chatting with clients in her native Portuguese, as well as Italian, Spanish, and English. She’s someone who cares, the type of person who snuck her clients a meal of pasta and homemade meatballs, before the rule that PSWs could only make sandwiches or heat up food.
She tried to think back to when she could have been exposed and remembered visiting a client a week earlier whose wife looked pale and was coughing. Gilbert had called ahead and screened her clients for symptoms, as she’d been instructed to, but she wasn’t told to screen family members, and she can’t control who comes and goes from a house anyway.
As soon as she developed symptoms, Gilbert stopped working. She doesn’t get sick days—the base two sick days that had been instituted for all workers by the previous provincial government were swiftly taken away when the Conservatives came to power. So she’s on EI, earning less than $2,000 a month. She’s been trying to stay away from her teenage sons to keep them safe and is often too exhausted to convince them to put away their video games. “The noise, it’s driving me crazy,” she says. Their apartment near Keele and Eglinton has one bathroom, so every time she uses it, she wipes down all the surfaces.
On Wednesday, three weeks after first getting sick, Gilbert still hadn’t fully recovered. She was eating half of what she normally does and was still easily exhausted. She also still hadn’t been tested for the virus. Her family doctor told her in March to only go to a COVID-19 clinic if her situation worsened, as tests were being rationed. She’s asked her employer more than once to follow up with her clients, to trace the potential source and protect other workers, but to her knowledge that hasn’t happened. Gilbert isn’t surprised by the lack of vigilance. She says friends of hers who had been providing drop-in care at a long-term care home weren’t told that one of their daily clients had been tested for COVID-19 until days later. “We’re being treated like ragdolls,” she says.
PSWs like Gilbert are essential to our health system. They allow those who want to remain in their homes to do so, freeing up space in our strained long-term care system and hospitals. They take care of wounds so they don’t become infected and raise the alarm about deteriorating cognitive functions. In other words, they ensure health conditions don’t become emergencies. They’re “the front of the frontline,” says Miranda Ferrier, president of the Ontario Personal Support Workers Association. But they’re undervalued, perhaps because their contributions are invisible, taking place behind closed doors in private homes, or perhaps because they’re almost all women, and many are immigrants who speak English as a second language.
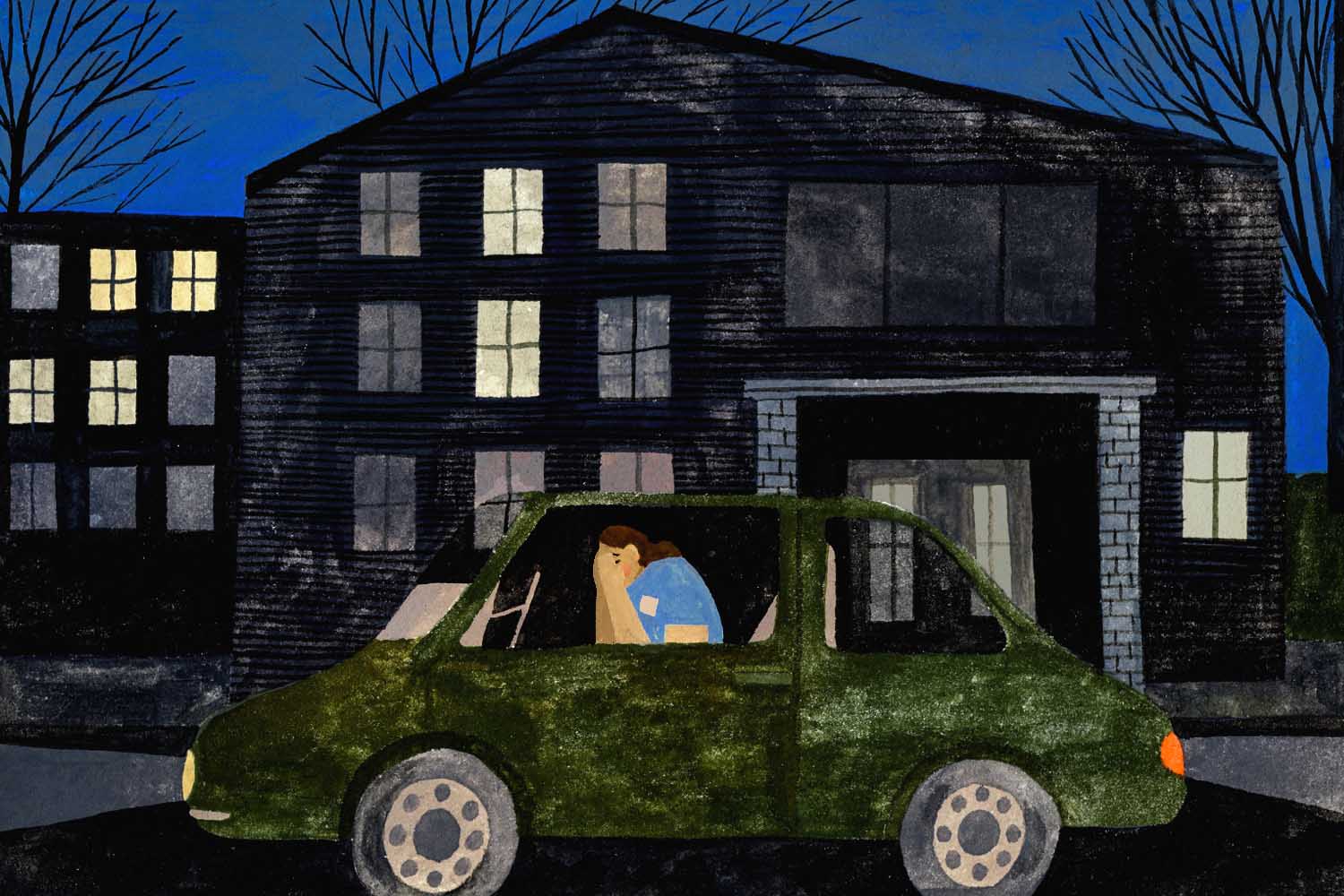
Now, with COVID-19, their situation is worsening. They’re making less money, as their hours are being cut by families that understandably want to limit exposure from a travelling PSW. And at long-term care homes, they’re working harder, disinfecting surfaces, worried constantly about getting the virus and bringing it home. Some call Ferrier in their cars outside of homes, crying, worried about falling sick and passing on the virus to their children or aging parents. “We’re being seen as goats, as carriers,” says Gilbert. “When really, we’re victims.”
“Now all of a sudden they’re essential, but not essential enough to have sick time, not essential enough to have retirement savings or make a decent wage.”
As Gilbert mustered the energy to prepare food for her kids, across the city Gloria Turney was sorting out medications for one of her clients at a transitional care home in Burlington. Born in Jamaica, she’s been working as a PSW for 18 years, and she loves her job. “Every day, you feel like you make a difference,” she says. But these days are hard.
Normally, her clients aren’t here for more than a couple of weeks before they’re placed in a permanent long-term care home, but now it’s “no one in, no one out,” says Turney. Like so many, the residents have been in limbo since mid-March. Visitors, even close family members, aren’t allowed in. Turney notices that some of her clients have become depressed, and she’s worried about their health issues—an X-ray that is on hold, a wound that needs a doctor’s attention.
It seems like every day there’s a new protocol. Temperature checks, more surfaces to clean with virus wipes, new physical distancing measures. The care home has halved the number of residents who can be in the dining room at any one time, so that means two services for each meal, with cleaning in between. “There’s just more on you,” says Turney.
Tali Zrehen, director of home and community care at Service Employees International Union (SEIU), which represents 16,000 home care workers in Ontario, says that even before the pandemic, PSWs faced “a ton of health and safety problems and a lack of oversight.” With COVID-19, “these issues have been exacerbated to a breaking point for a lot of people.”
Adding to Turney’s list of worries is the fact that PSWs don’t have adequate personal protective equipment (PPE). In the transitional care home, which doesn’t currently have a positive case, Turney gets two surgical masks a day, plus a gown, gloves, and goggles. Gilbert says her colleagues are still only getting one mask a day. They’re wearing the same mask from home to home, and in many cases on public transit between clients.
And the nature of the work means that physical distancing isn’t possible. PSWs are bathing clients, doing diaper changes, providing medication, inserting suction tubes down throats. “They’re doing intimate, personal care,” says Zrehen. She says employers would like to offer more PPEs, but they don’t have access to the equipment. “The government has been focusing a lot on acute care and hospitals and lately long-term care homes, but not home and community care,” says Zrehen.
While the job has gotten harder and more dangerous, Turney is also getting fewer hours than she did before the pandemic. She normally provides care in people’s homes, but those clients have cancelled her services out of COVID-19 fears. Her income has been cut by a quarter. In home care, even employees with high seniority aren’t guaranteed hours. When clients cancel hours, PSWs can go from working 40 hours a week to 10, with no recourse, explains Zrehen.
On Wednesday, the Ontario government passed emergency legislation that forbids PSWs from working in more than one facility, as outbreaks of COVID-19 surge in around one sixth of the province’s long-term care facilities. The government has promised support for PSWs who will go down to part-time work because of this, but it’s not clear what that will look like.
Some PSWs would prefer to just take the emergency benefit or EI and avoid putting themselves and their families at risk of a potentially fatal virus. But last month, the Ontario government deemed PSWs essential, so they can’t refuse to work. It’s ironic, because SEIU has been fighting for years for PSWs to be determined essential, a designation that typically comes with much higher compensation and benefits. “Now all of a sudden they’re essential, but not essential enough to have sick time, not essential enough to have retirement savings, or make a decent wage,” says Zrehen.
PSWs start at $16.50 an hour. Both Gilbert and Turney are senior PSWs, so they’ve reached the maximum wage, $19 an hour. But it’s not enough, especially considering they’re not adequately compensated for travel time between clients. By Gilbert’s calculations, she loses almost three hours a day in unpaid time on transit, because her employer pays travel time according to how long it would take in a car. “Every day, you hear about the frontline worker, ‘We thank you, we thank you,’” says Turney. But while grocery workers are getting a raise, and other frontline employees like police officers are getting one-time bonuses due to the additional risk, many PSWs are effectively seeing a salary cut.
Ferrier wants to make it clear that PSWs are more than willing to do their part. “We have PSWs working in long-term care homes who are self-isolating away from their families,” says Ferrier, who recently sent take-out to a house that four PSWs are temporarily sharing to avoid spreading the disease to their loved ones. In other cases, PSWs who have seen their home care clients dry up have taken on temporary contracts in long-term care homes that are short-staffed because of outbreaks. On Friday, Christine Mandegarian, a PSW working in a Scarborough nursing home, became the first PSW to die from COVID-19. “They’re marching in droves towards the front of the frontlines of health care,” says Ferrier.
“We’re being seen as goats, as carriers. When really, we’re victims.”
On Wednesday, Turney visited one of her favourite clients at the transitional home, a woman we’ll call Rose. Amid the difficulties of the last weeks, Rose, who is in her 90s, has been a bright light. When Turney rubbed lotion on her face a couple of weeks ago, Rose told her she was so good, she would pay $100,000 for her make-up business. Now it’s a running joke between the two of them. When Turney asks about her start-up capital, Rose always has a quick response—“didn’t I give it to you yesterday?”
Today, Rose has a missed call, so Turney hits the missed FaceTime icon on her phone. A series of smiling faces pop up, Rose’s children and their partners, but this time they want to talk to Turney. They want to thank her for the care she’s providing, for the way she’s keeping Rose connected to them. They tell her there are flowers waiting at the front desk.
Both Turney and Gilbert love their work. Gilbert got into the profession when her father was dying of cancer and she realized how important it was to provide comfort and dignity in people’s final years. She fiercely advocates for her clients, demanding more hours or long-term care placements for those who need it.
Turney can’t imagine walking away from her clients. Often, she’s their only source of human touch in a day. “They’re saying, ‘When will this be over? When can my children come in?’” she says. “Every day you have to reassure them that this too shall pass… you have to be strong about it because you can’t go in and show your fears.”







